By: Daniel Millard, PhD
Today's Clinical Lab, 2022
The success of any adoptive cell therapy (ACT) depends on its ability to efficiently and effectively kill tumor cells without eliciting severe adverse effects in patients. Before a treatment reaches the clinic, it is up to translational research labs to assess the cytotoxicity of these experimental therapies and identify candidates that are most likely to meet specific quality criteria in clinical trials and beyond. To help accomplish this, these labs use cell viability assays.

A cell viability assay enables researchers to identify whether cells have survived exposure to a treatment or other environmental change. For decades, researchers have used cell viability assays to test everything from the effects of cryopreservation to the toxicity of novel drug candidates. In the last decade, these assays have taken on a new application: measuring the cytotoxicity of ACTs.
Clinical researchers seeking to develop novel ACTs face several challenges. Most importantly, ACTs are “living drugs” that operate by their own biological processes, making their development and behavior relatively unpredictable compared to small molecule drugs. As a result, researchers need to rethink which cell viability assay will offer the information they need to assess a novel therapy before it reaches patients.
This article will describe five popular cell viability assays and their benefits and limitations in the context of ACT development:
1. Chromium release assays
Historically, the chromium release assay has been widely used to measure the cytotoxicity of ACTs. This assay has stood the test of time because it is relatively easy to perform. Researchers load target cells with 51Cr, a radioactive marker, and then apply their effector cells and measure the radioactive chromium as it leaks from the dying cells. The recorded radiation directly correlates with cell death.
Despite its simplicity, the chromium release assay is not ideal for studying ACTs due to its many limitations:
First, the assay can only measure cell death at one point in time, meaning researchers cannot measure the kinetics of cell death in response to treatment. This limitation reduces the volume of information researchers can collect about the quality of a therapeutic agent.
Second, the assay poses a health hazard. Organizations often require that researchers limit their exposure to radioactive materials and users need special training on how to handle radioactive materials to be able to run a chromium release assay.
Third, these assays are not cheap to run. To measure radioactivity, researchers need to purchase an expensive gamma counter and it takes additional effort and money to safely dispose of radioactive waste. In recent years, researchers have turned to safer, cheaper, and more flexible cell viability assays.
2. LDH assays
Since this assay measures a natural component of cells, researchers do not need to use fluorescence or genetic manipulations to measure cell viability. As such, LDH assays are not destructive to the specimen, making them ideal for measuring the viability of small or limited samples.
Researchers measure LDH by quantifying the product of a secondary interaction initiated by LDH. LDH catalyzes the production of pyruvate, which interacts with a tetrazolium salt to form a red molecule that can be quantified using colorimetry. As more cells die, and more LDH is released, more red molecules are produced. But like chromium release assays, LDH assays can only measure cell viability at one point in time and don’t provide enough information to determine a therapy’s quality with certainty.
3. MTT assays
MTT and related molecules are a measure of mitochondrial activity, a sign of cell viability. Like LDH assays, MTT assays indicate cell viability using colorimetry rather than by emitting radiation. Mitochondria convert MTT into purple crystals, and researchers can measure the intensity of the purple color using a spectrophotometer. When cells start dying, their mitochondria slow down, and the reaction stops. Therefore, the less intense the purple color, the more toxic the effector cells.
Although MTT and LDH assays are non-toxic and cheap, these methods still do not overcome the primary limitation that hampers their ability to profile the cytotoxicity of ACTs: they only measure cell death at one point in time. Furthermore, although researchers generally agree that the assay is relatively straightforward, some question its accuracy and precision due to the number of potentially confounding variables. As such, these assays are not ideal for monitoring the cytotoxicity of cells designed to treat humans, where accuracy and precision are especially important.
4. Live-cell imaging
ACT researchers need to analyze time-dependent events such as peak killing rate, T-cell exhaustion, and signs of chronic activation. As discussed, chromium, LDH, and MTT assays offer incomplete information about the quality of ACTs, limiting researchers’ ability to accurately characterize a therapy.
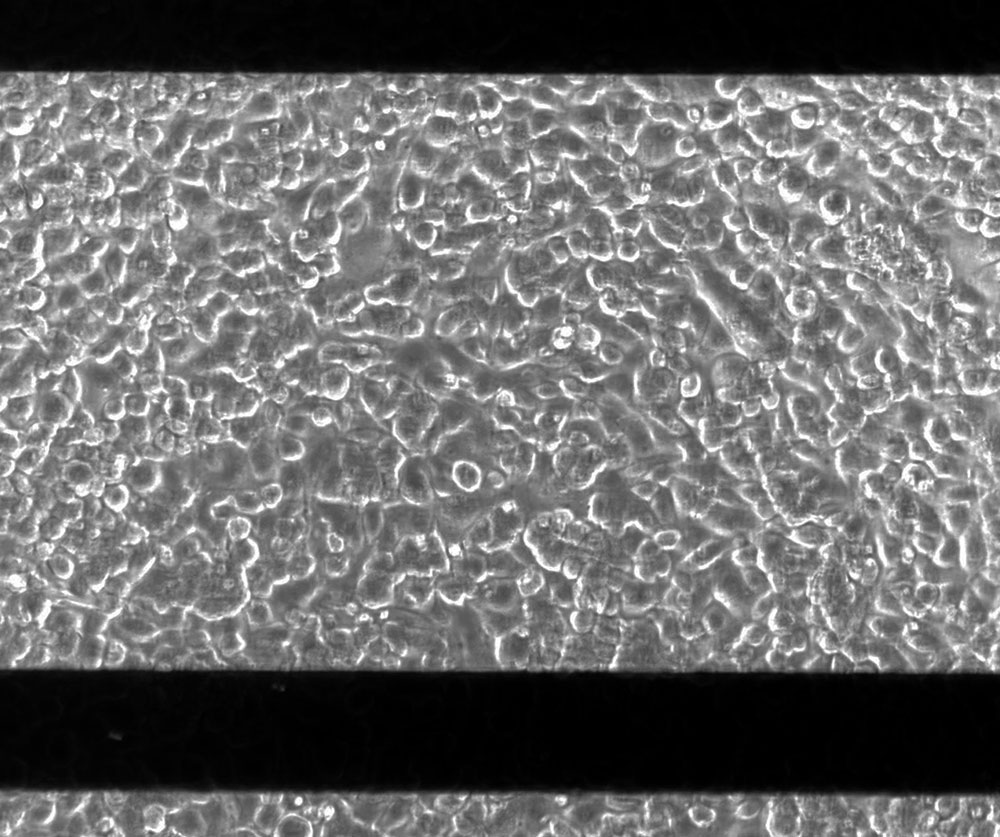
With live-cell imaging, researchers can overcome this limitation. Live-cell imaging uses microscopy to visualize ACT dynamics over time. Researchers can examine activity over hours to weeks and capture all critical time points without any guesswork.
But when it comes to testing ACTs, live-cell imaging presents its own challenges. For example, researchers first plate target cells and then place their effector cells on top, potentially obscuring the view and making it difficult to accurately measure cytotoxicity. Researchers can thus use dyes to distinguish between the two cell layers, but this extra step can sometimes disturb the activity of the effector cells and disrupt the results. Finally, given the subjectivity inherent in analyzing visual data, monitoring cells for signs of cell death requires a trained eye.
5. Impedance monitoring with a bioelectronic assay
Bioelectronic assays allow researchers to monitor cell viability using sensitive bioelectrodes to detect cell death in real time without dyes, labels, or probes that can interfere with the data.
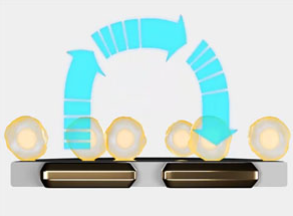
For this type of assay, the bioelectrodes are embedded in the bottom of each well in a multiwell plate. Researchers add the target cancer cells and give them time to grow and attach to the surface. As they cover the surface, the target cells impede electrical signals between electrodes. Then, researchers apply the effector immune cells. As the effector cells start killing the target cells, the target cells lyse or detach, and the impedance between electrodes decreases. Since immune cells are nonadherent, they are not a significant source of impedance relative to target cells, making the assay very sensitive to target cell death.
Unlike chromium release, MTT, and LDH assays, bioelectronic assays allow researchers to monitor the dynamics of ACT-induced cell killing in real time to monitor the nuances of their behavior. And in contrast to live-cell imaging, the results are objective; the bioelectrodes collect the data directly and there is no visual data a researcher must be trained to interpret accurately. Future researchers can use these data to develop better ACT products for use in people.
Recently, Lohitash Karumbaiah, PhD, associate professor at the University of Georgia, measured impedance to characterize a novel CAR-T cell therapy designed to treat glioblastoma. His group observed that their CAR-T cells performed significantly better than naive T cells in killing glioblastoma cells in vitro. The researchers’ impedance assay could measure the effects of several doses at once, and it was sensitive enough to detect cell death when treated with the smallest concentration of CAR-T cells. This research may contribute to developing novel treatments for glioblastoma—the deadliest form of brain cancer.
Selecting the best cell viability assay for your lab
ACTs have changed cancer therapy, but the therapy still has a long way to go. Countless patients are waiting for an ACT to treat their cancer, and researchers are working hard to engineer safe and effective cells to meet the demand.
But ACTs are not like typical drugs or treatments, and their quality cannot be assessed using typical assays. Instead, assessing ACTs requires tools that can handle the variability that comes with designing treatments made with living cells. Bioelectronic assays offer the objectivity, quantitative ability, accuracy, and exhaustiveness needed to profile ACTs to the extent necessary for regulatory approval and use in patients.



