Manufacturing Chemist, 2021
Cell-based immunotherapies are revolutionising medicine; and, although they are relatively new, they are poised to disrupt the biomedical industry, reports Dr Jim Ross, Chief Technology Officer and cofounder, Axion Biosystems
Researchers are rapidly developing new cell therapies and working to discover new drug targets, both of which are fuelling rapid growth in this market.
However, scientists need superior assays to understand how the living cells involved in these therapies function in real-time. Impedance-based cell analysis is a well-established technique to monitor the presence, morphology and behaviour of cells in culture.
This methodology allows scientists to non-invasively measure the tumour-killing activity of CAR-T cells and other cell-based immunotherapies in a dish in real-time without labels or dyes. This precise, continuous monitoring opens the door to new ways of studying some of the world’s most challenging diseases.
Use cases to discover new targets
Glioblastoma (GBM), also referred to as grade IV astrocytoma, is a fast-growing and aggressive brain tumour that is a particularly challenging form of cancer.
According to the American Association of Neurological Surgeons, GBMs comprise the most common malignant brain and other CNS tumours, accounting for 47.7% of all cases.1
GBM has no effective treatments and a prognosis of only 12–15 months. GBMs present unique treatment challenges owing to the localisation of tumours in the brain, inherent resistance to conventional therapy, the migration of malignant cells into adjacent brain tissue and the resultant neurotoxicity of treatments directed at gliomas. Consequently, patients are in urgent need of new therapeutic approaches that can improve clinical outcomes.
Cancer immunotherapy for GBM
Cancer immunotherapies harness the innate power of the immune system to fight cancer. One such therapy is chimeric antigen receptor (CAR)-T cell therapy, a form of targeted immunotherapy that involves the modification of T cells to target specific antigens expressed on the tumour cell surface.
CAR-T cell therapies have demonstrated great success against lymphoma and leukaemia; however, similar success against GBM has not yet been achieved. But now, novel CAR-T cells are being developed to better target GBM.
Researchers need tools that can safely and accurately model the activity of CAR-T cells against human tissue and tumours. Recent findings demonstrate the value of using an in vitro impedance-based assay to assess therapeutic CAR-T cell potency against glioblastoma.
In vitro assessment
Although the in vivo assessment of CAR-T cell therapy function can be complex and difficult to accomplish safely, in vitro assays such as the bioelectronic cell impedance assay provide useful, applicable insights into the targeting potency of CAR-T cells.
The in vitro impedance assay is a powerful tool that can accelerate investigations into therapeutic cell efficacy and identification of desirable quality attributes.
Bioelectronic assays provide a sensitive, label-free, non-destructive method to continuously monitor cancer cell proliferation and immune-mediated cytotoxicity.
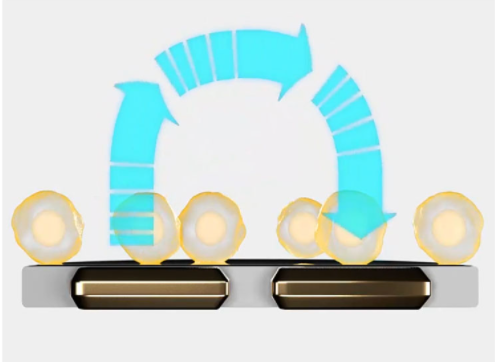
Using small currents from electrodes embedded in the well, the opposition to current flow from one electrode to another defines the impedance of the cell-electrode interface (Figure 1). When cells are present and attached to the substrate, they block these electrical currents and are detected as an increase in impedance.
Impedance is sensitive to many aspects of cell behaviour: attachment, spreading, shape, cell-cell connections (tight junctions) and death. Even small, transient changes such as swelling or signalling are detectable by impedance.
Because impedance is non-invasive and label-free, the dynamics of these changes can be monitored in real-time for minutes, hours or even days without disturbing live biological samples.
Scientists can reduce their dependence on laborious endpoint assays such as the chromium release test or various colorimetric analyses that quantify cytotoxicity at a single time point and require dyes and labels with their own optimisation or safety protocols. Bioelectronic assays may be run without specialised training, using only basic cell culture techniques.
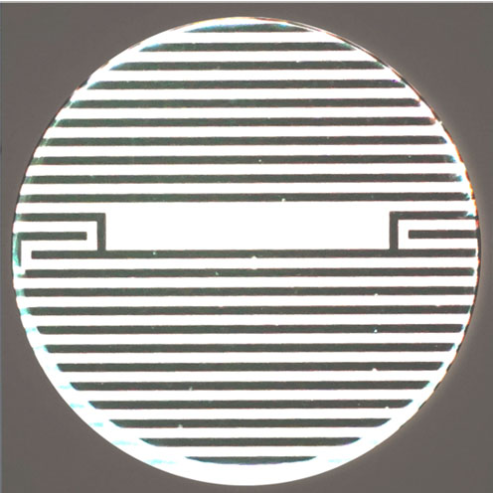
For instance, Axion Biosystems’ 96-well CytoView-Z plate has electrodes embedded in the culture surface of each well (Figure 2), so a scientist only has to culture target cancer cells in the plate and load it into the Maestro Z bioelectronic assay system.
The environmental chamber automatically equilibrates to the desired conditions and the system automatically monitors target cell attachment and proliferation.
When T cells are added, T cell-mediated target cell killing can be tracked in real-time. This streamlined process provides a powerful means of assessing CAR-T potency.
Alternatives to in vivo assessment with impedance assays
This technology is already proving its usefulness: Dr Lohitash Karumbaiah, Associate Professor of Regenerative Medicine at the University of Georgia, used label-free impedance measurements to assess the potency of human CAR-T cells against glioblastoma stem cells (GSCs).2
Karumbaiah and his team assessed the expression level of several popular CAR-T targets in patient-derived GSCs, identifying GD2 as significantly higher than many others.
After plating the GSCs, the researchers continuously monitored impedance with the Maestro Z system as the cells attached and proliferated. After 50 hours, CAR-T cells or untargeted naive activated T cells were added at various effector:target cell ratios.
Karumbaiah and his team observed that both the addition of GD2-targeted CAR-T cells and naive T cells to GSC cultures resulted in pronounced cell death, indicated by a progressive reduction of cellular impedance when compared with untreated controls across all ratios. This result was consistent with the immune cell-mediated lysis of glioblastoma stem cells.
Although untreated GSC wells continued to increase in impedance as the cancer cells proliferated with time, both types of effector cells induced cell death at all ratios. Karumbaiah and his team were able to observe immune cell-mediated cytotoxicity by tracking percentage cytolysis in real-time.
They found that GD2-targeted CAR-T cells showed significantly higher cytolysis in 7 days compared with naive T cells and different effector:target ratios lead to different kinetics of the cytotoxic response, which can all be accurately tracked and measured with a bioelectronic assay.
Conclusion
Overall, impedance-based cytotoxicity assays provide many advantages for the examination of T-cell and cancer cell interactions to support the progress of CAR-T cell research.
The researchers found a high sensitivity over various effector:target cell ratios in a method that provides label-free and real-time monitoring. Furthermore, bioelectronic assay systems give scientists the ability to precisely control environmental conditions to conduct physiologically relevant and reproducible experiments with translational impacts.
The data generated using these experiments demonstrates how impedance technology and bioelectronic assays can inform cell-based assays on CAR-T cell targeting and efficacy for solid tumours.
By helping scientists to make new breakthroughs in drug discovery, this technology has the potential to revolutionise the future of biomedical research.
References
- www.aans.org/en/Patients/Neurosurgical-Conditions-and-Treatments/Glioblastoma-Multiforme.
- www.axionbiosystems.com/resources/video/kinetics-and-potency-gd2-car-t-cell-mediated-cytolysis-glioblastoma.



